3-D Printed Heart Valve Models Honored in International Competition
Dec 21, 2018 — Atlanta, GA

Inside the 3-D printed model of a human heart valve, black regions represent the location of actual calcium deposits. (Credit: Rob Felt, Georgia Tech)
A Georgia Institute of Technology and Piedmont Heart Institute project to create tissue-mimicking heart valve models using advanced 3-D printers has been named one of the best new technologies of the year in an international research and development competition.
The project was among the recipients of the 56th annual R&D 100 Awards, which recognize the best 100 technologies of the year as judged by the publishers of R&D Magazine.
The heart valve models were designed to assist cardiologists during pre-surgery preparations for life-saving heart valve replacements. The researchers used patient imaging to create models with the same dimensions and physical characteristics of the patient’s real valve.
“With evolving additive manufacturing technologies, it will be possible to fabricate ‘plastic tissues’ with both accurate anatomical and biomechanical properties unique to each patient’s biomechanical & pathological characteristics,” said Chuck Zhang, Harold E. Smalley Professor in the Stewart School of Industrial and Systems Engineering at Georgia Tech.
The aim of the project was to improve the success rate of transcatheter aortic valve replacements (TAVR). Tens of thousands of patients each year are diagnosed with heart valve disease, and TAVR is often considered for patients who are at high risk for complications with an open-heart surgery to replace the valve.
The prosthetic valves are made in a variety of sizes from multiple manufacturers. Leakage occurs when the new valve doesn’t achieve a precise fit and blood flows around the prosthetic rather than through it as intended. Reducing the chances for leakage is key to a good patient outcome for the procedure.
The models created by the Georgia Tech-Piedmont team could allow doctors in pre-surgery planning to test different prosthetic valves and pick the right prosthetic and identify the best placement to avoid leakage.
“Patient-specific tissue-mimicking models have a wide range of biomedical applications, including validation of computational models and imaging techniques, medical device testing, surgery planning, and medical education and training,” said Ben Wang, executive director of the Georgia Tech Manufacturing Institute (GTMI) and the Eugene C. Gwaltney Jr. Chair in Manufacturing Systems for the H. Milton Stewart School of Industrial and Systems Engineering.
The models were created with a special metamaterial design, and then made by a multi-material 3-D printer, which gives the researchers control over such design parameters as diameter and curving wavelength of the metamaterial used for printing, to more closely mimic physiological properties of the tissue.
For example, the models can recreate conditions such as calcium deposition – a common underlying factor of aortic stenosis – as well as arterial wall stiffness and other unique aspects of a patient’s heart.
Last year, the research team published results from their tests in the journal JACC: Cardiovascular Imaging, reporting that the models behaved so similarly to the real ones that they could reliably predict the leakage.
“This process provides high value for advanced medical device development and surgery planning,” said Kan Wang, a research engineer at GTMI. “It could someday be a standard tool to help physicians with these procedures.”
The R&D 100 Awards were announced Nov. 16 in Orlando, Fla.
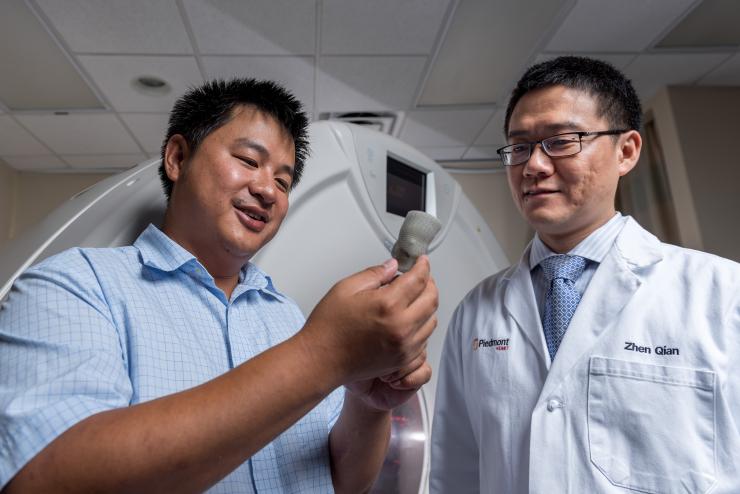
Kan Wang, a postdoctoral researcher at Georgia Tech, and Zhen Qian, chief of cardiovascular imaging research at Piedmont Heart Institute, inspect a printed heart valve. (Credit: Rob Felt, Georgia Tech)

New 3-D printing technologies allow researchers to create patient-specific heart valve models that mimic the physiological qualities of the real valves. This image shows the submerged valve during flow testing. (Credit: Rob Felt)

Chuck Zhang, Harold E. Smalley Professor in the Stewart School of Industrial and Systems Engineering at Georgia Tech, in Orlando, Fla., to receive the R&D 100 Award.
Research News




