Apr. 15, 2020
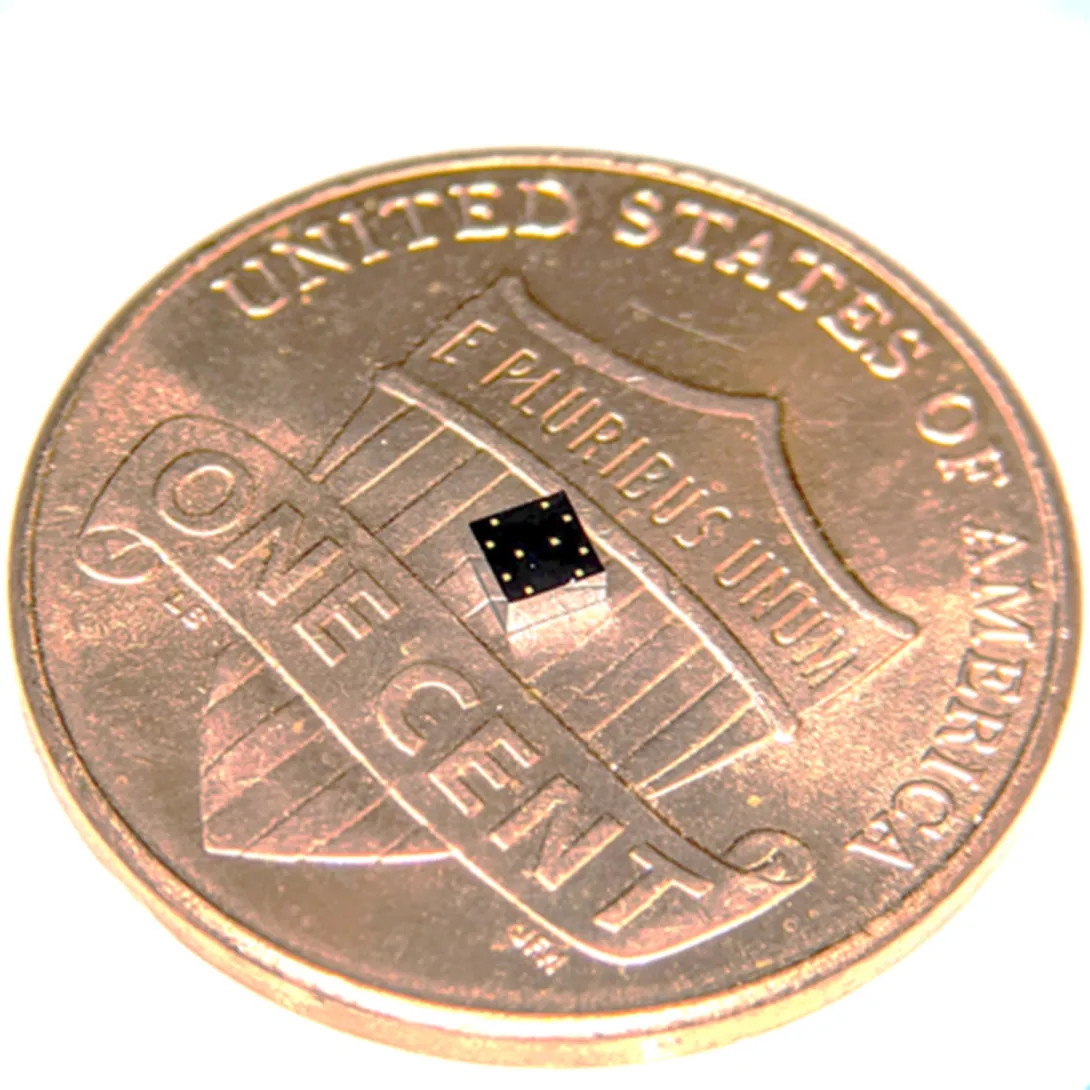
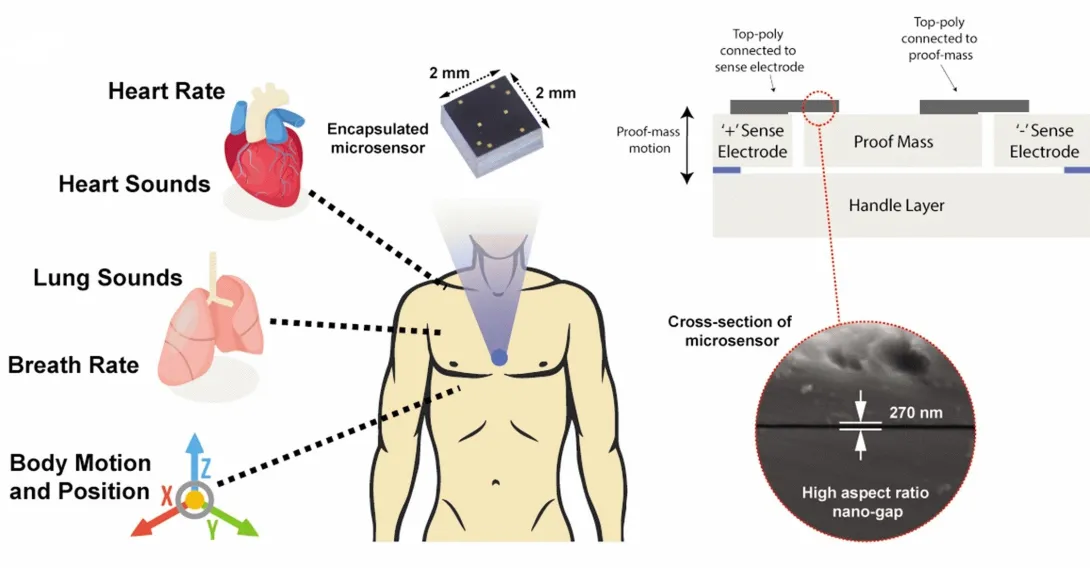
During a stroll, a woman’s breathing becomes a slight bit shallower, and a monitor in her clothing alerts her to get a telemedicine check-up. A new study details how a sensor chip smaller than a ladybug records multiple lung and heart signals along with body movements and could enable such a future socially distanced health monitor.
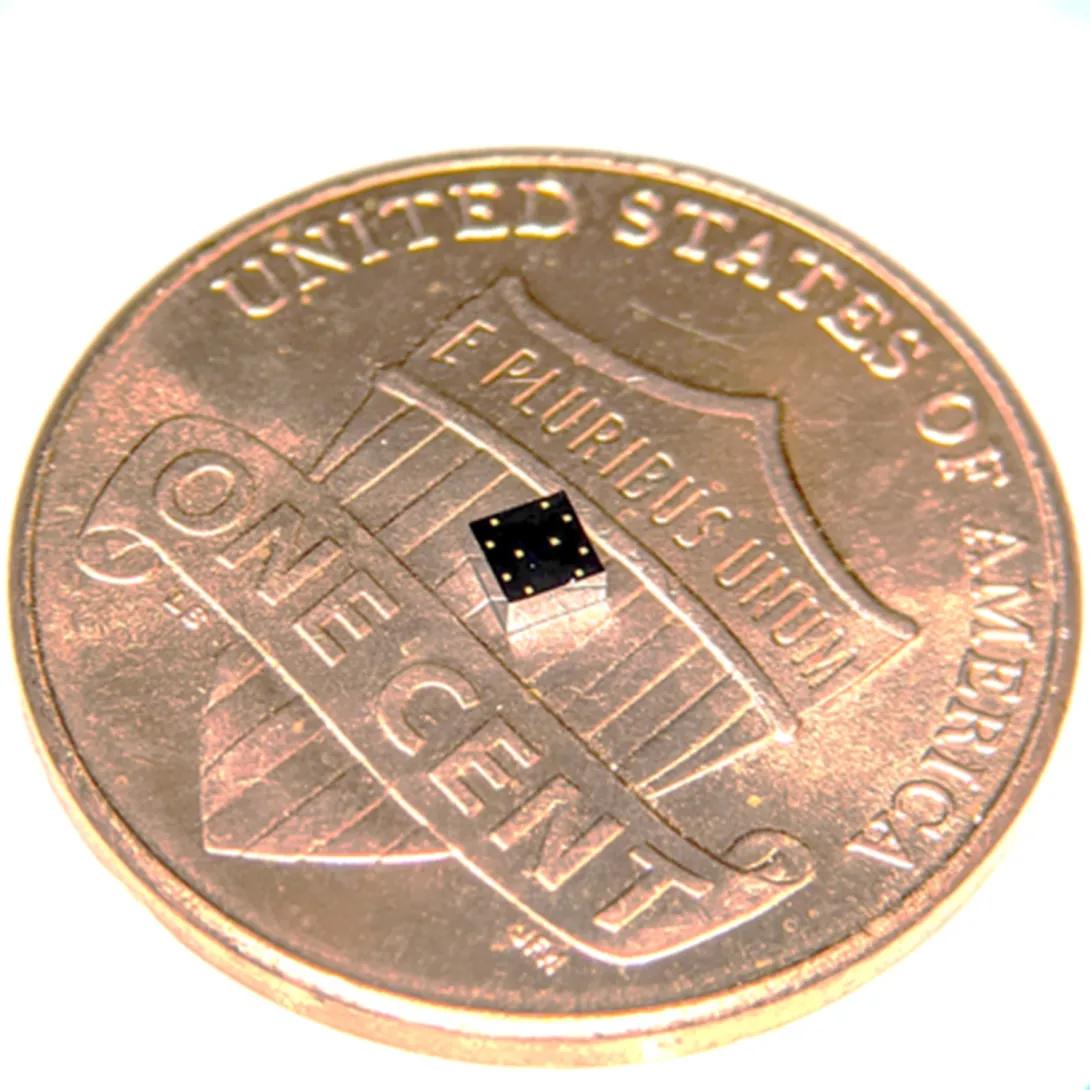
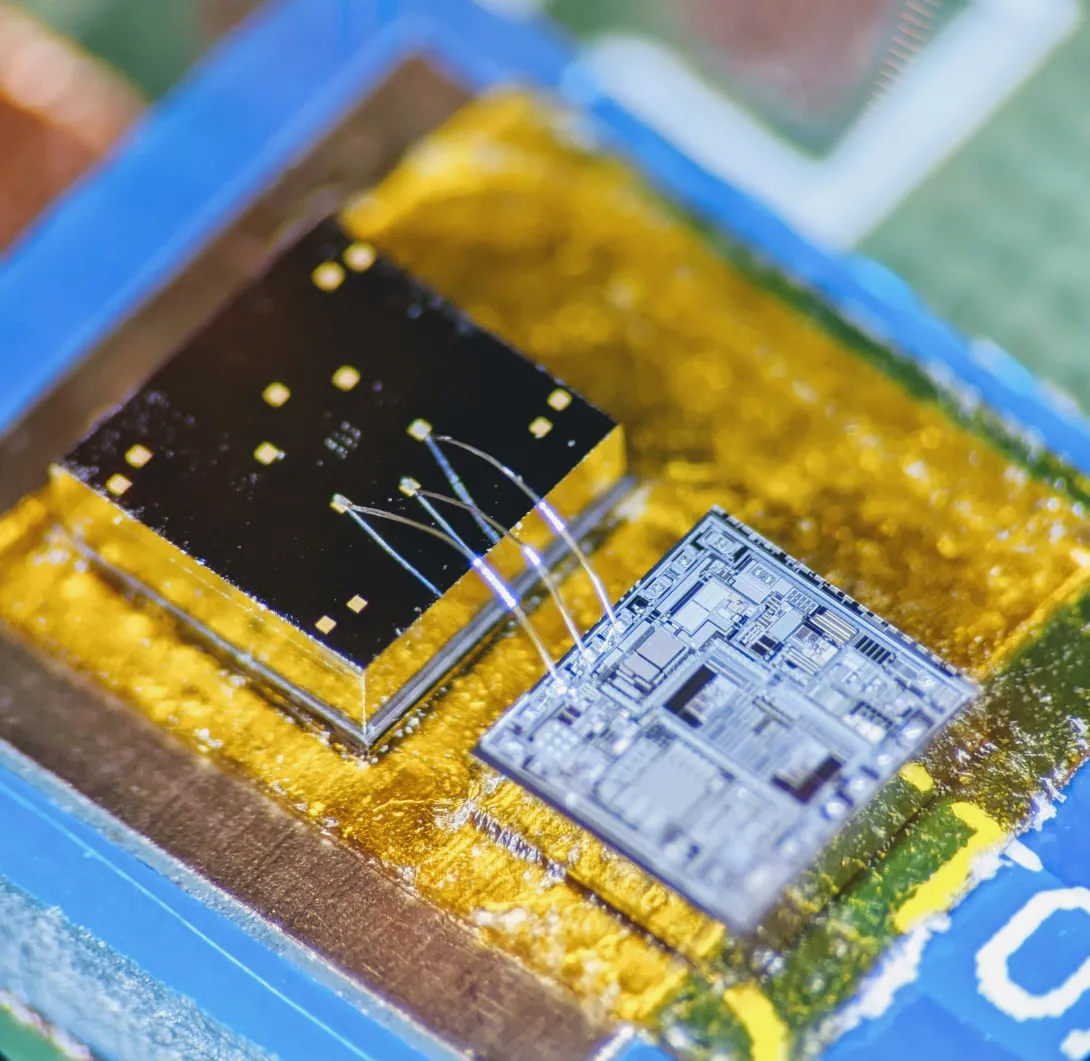
The core mechanism of the chip developed by researchers at the Georgia Institute of Technology involves two finely manufactured layers of silicon, which overlay each other separated by the space of 270 nanometers – about 0.000001 inches. They carry a minute voltage.
Vibrations from bodily motions and sounds put part of the chip in very slight motion, making the voltage flux, thus creating readable electronic outputs. In human testing, the chip has recorded a variety of signals from the mechanical workings of the lungs and the heart with clarity, signals that often escape meaningful detection by current medical technology.
“Right now, medicine looks to EKGs (electrocardiograms) for information on the heart, but EKGs only measure electrical impulses. The heart is a mechanical system with muscles pumping and valves opening and shutting, and it sends out a signature of sounds and motions, which an EKG does not detect. EKGs also say nothing about lung function,” said Farrokh Ayazi, Ken Byers Professor in Georgia Tech’s School of Electrical and Computer Engineering.
Stethoscope-accelerometer combo
The chip, which acts as an advanced electronic stethoscope and accelerometer in one, is aptly called an accelerometer contact microphone. It detects vibrations that enter the chip from inside the body while keeping out distracting noise from outside the body's core like airborne sounds
“If it rubs on my skin or shirt, it doesn’t hear the friction, but the device is very sensitive to sounds coming at it from inside the body, so it picks up useful vibrations even through clothing,” Ayazi said.
The detection bandwidth is enormous - from broad, sweeping motions to inaudibly high-pitched tones. Thus, the sensor chip records all at once fine details of the heartbeat, waves the heart sends through the body, and respiration rates and lung sounds. It even tracks the wearer’s physical activities such as walking.
The signals are recorded in sync, potentially offering the big picture of a patient’s heart and lung health. For the study, the researchers successfully recorded a “gallop,” a faint third sound after the “lub-dub” of the heartbeat. Gallops are normally elusive clues of heart failure.
The researchers published their results in the journal npj Digital Medicine on February 12, 2020. The research was funded by the Georgia Research Alliance, the Defense Advanced Research Projects Agency (DARPA), the National Science Foundation, and the National Institutes of Health. Study coauthor Divya Gupta, M.D., a cardiologist at Emory University, collaborated in testing the chip on human participants.
Hermetically sealed vacuum
Medical research has tried to make better use of the body’s mechanical signals for decades but recording some – like waves traversing multiple tissues – has proven inconsistent, while others – like gallops – have relied upon clinician skills influenced by human error. The new chip produces high-resolution, quantified data that future research could match to pathologies in order to identify them.
“We are working already to collect significantly more data matched with pathologies. We envision algorithms in the future that may enable a broad array of clinical readings,” Ayazi said.
Though the chip’s main engineering principle is simple, making it work and then manufacturable took Ayazi’s lab ten years, mainly because of the Lilliputian scale of the gap between the silicon layers, i.e. electrodes. If the 2-millimeter by 2-millimeter sensor chip were expanded to the size of a football field, that air gap would be about an inch wide.
“That very thin gap separating the two electrodes cannot have any contact, not even by forces in the air in between the layers, so the whole sensor is hermetically sealed inside a vacuum cavity,” Ayazi said. “This makes for that ultralow signal noise and breadth of bandwidth that are unique.”
Detects through clothing
The researchers used a manufacturing process developed in Ayazi’s lab called the HARPSS+ platform (High Aspect Ratio Poly and Single Crystalline Silicon) for mass production, running off hand-sized sheets that were then cut into the tiny sensor chips. HARPSS+ is the first reported mass manufacturing process that achieves such consistently thin gaps, and it has enabled high-throughput manufacturing of many such advanced MEMS, or microelectromechanical systems.
The experimental device is currently battery-powered and uses a second chip called a signal-conditioning circuit to translate the sensor chip’s signals into patterned read-outs.
Three sensors or more could be inserted into a chest band that would triangulate health signals to locate their sources. Someday a device may pinpoint an emerging heart valve flaw by turbulence it produces in the bloodstream or identify a cancerous lesion by faint crackling sounds in a lung.
Here's how to subscribe to our free science and technology newsletter
Also read: Digital tool helps with tough COVID19 decision
These researchers co-authored the study: Pranav Gupta (first author), Mohammad Moghimi, Yaesuk Jeong and Omer Inan from Georgia Tech. The research was funded by the Georgia Research Alliance, the Defense Advanced Research Projects Agency (DARPA) Technology Office’s Advanced Inertial Micro Sensors program (contract # N66001-16-1-4064), and by the National Science Foundation/National Institutes of Health Smart and Connected Health Program (grant # R01 EB023808). The team’s work with human subjects was approved by Emory University and Georgia Institute of Technology Institutional Review Boards (IRB# H18248). Any findings, conclusions or recommendations are those of the authors and not necessarily of the sponsors.
Writer & Media Representative: Ben Brumfield (404-272-2780), email: ben.brumfield@comm.gatech.edu
Georgia Institute of Technology
Apr. 14, 2020
What-if questions can torment a doctor making coronavirus retest decisions: What if a patient’s initial negative test was a false negative, and he or she needs a second test? What if they don’t need it, and a retest would use up a scarce test kit and treatments that other patients need?
Such challenges led Piedmont Healthcare in Atlanta to establish a paper-based decision tree for ordering COVID-19 retests, and researchers at the Georgia Institute of Technology turned it into an automated digital tool. Piedmont further developed the tool and has now built it into the hospital’s electronic medical record, where it influences the ordering of retests.
A user can answer their “ifs” by clicking through questions, and the “if-this-then-do-that” algorithm makes recommendations for best courses of action, ranging from immediately treating a patient for COVID-19 to retesting to consulting a specialist. The final decision remains with the physician.
The questions are deceptively simple, but the recommendations are not always obvious. That reflects the algorithm’s usefulness to fill gaps in thinking about the new sickness, which can confront clinicians with surprises.
“If a patient has not had close contact with positive patients and the first test came back negative, a physician may think the patient does not need to be retested. But actually, the patient may need a second test because they are in intensive care and also have suspicious chest X-rays,” said Georgia Tech graduate research assistant April Yu, who converted the decision tree into a digital tool.
“One of our big worries in using a brand-new test like the coronavirus test is that it will miss real cases, and this tool helps prevent that,” said Dr. Bronwen Garner, who helped develop the original decision tree and is an infectious disease specialist at Piedmont Healthcare. “It also helps reassure physicians when they get a negative result that it is probably a true negative.”
Suspenseful decision-making
A physician’s reaction to an initial negative test can mean life or death because the physician not only decides on follow-up testing but also on treatment pathways and quarantine.
“If you make a misstep in the thought process, it can lead to cascading impacts not only for the patient but also for healthcare professionals and family members, who may be exposed to the patient,” said Pinar Keskinocak, William W. George Chair and Professor in Georgia Tech’s Stewart School of Industrial and Systems Engineering. “This tool is meant to help doctors easily stay on the decision tree path.”
Michael O’Toole, executive director of Piedmont Healthcare’s quality improvement department, originally pictured doctors getting an automated version of the decision tree to use on their phones. O’Toole called Keskinocak, and she tapped Yu, a member of her research group.
“Literally within four hours they had it ready for us. It was incredible,” said O’Toole, a Georgia Tech alumnus who studied industrial and systems engineering.
“It was a very pleasant surprise,” said Dr. Garner, who is also a Georgia Tech graduate. “Automated tools are better than a paper format because they’re in the same format as orders in our electronic system. We get notifications in real time instead of having to remember to check a piece of paper.”
The tool is in place in the system where doctors order retests and is specific to Piedmont’s workflow. It may not be directly transferable to other health care systems.
Piedmont Healthcare simplified the logic even more, and the hospital built its own custom alerts to guide physicians on retesting. For cases that are more ambiguous, Piedmont Healthcare’s final version of the tool also gives physicians inside the hospital guidance to consult with their in-house infectious disease specialists.
If-this-then-retest
In her original version, Yu had turned the decision tree criteria into a short panel of questions with yes and no answers. It took her six iterations to arrive at her final version.
Yu’s version asked whether the patient:
- has a relevant ailment
- previously tested positive for coronavirus
- is now in an intensive care unit
- has worsening lung conditions
- shows telltale lung damage in imaging
- has been diagnosed with a different ailment
- the patient has had contact with someone else who tested positive for coronavirus.
On the back end, the algorithm guided the user through risks of coronavirus presence based on the answers.
“The steps were easy to follow, and the answers were color-coded for urgency with white, yellow, and red,” said Keskinocak, who also directs Georgia Tech’s Center for Health and Humanitarian Systems.
One bright yellow answer read: “This patient needs re-testing 24 hours after the initial test!” And there were further recommendations on how to handle the case.
Here's how to subscribe to our free science and technology newsletter
Also read: Advice on DIY masks
Writer & Media Representative: Ben Brumfield (404-272-2780), email: ben.brumfield@comm.gatech.edu
Georgia Institute of Technology
Apr. 13, 2020
Georgia Tech Arts is still seeking projects for the 2021 ACCelerate: ACC Smithsonian
Creativity and Innovation Festival in Washington, DC. All Georgia Tech students, faculty, and staff are invited to apply by May 1, 2020.
Even if you do not have a finished project exploring the intersection of science,
engineering, art, design, and technology, we encourage you to speak with Es
Famojure at esther.famojure@arts.gatech.edu about your concepts.
Learn about Georgia Tech's 2019 participants for some inspiration.
The festival brings together all institutions included in the Atlantic Coast Conference to
celebrate creativity and innovation with a specific focus on science, engineering, arts, and
design. It will be held April 9 -11, 2021 at the Smithsonian National Museum of American
History.
Submit your project for consideration by May 1, 2020 to be considered.
News Contact
Es Famojure
esther.famojure@arts.gatech.edu
Apr. 13, 2020
What-if questions can torment a doctor making coronavirus retest decisions: What if a patient’s initial negative test was a false negative, and he or she needs a second test? What if they don’t need it, and a retest would use up a scarce test kit and treatments that other patients need?
Such challenges led Piedmont Healthcare in Atlanta to establish a paper-based decision tree for ordering COVID-19 retests, and researchers at the Georgia Institute of Technology turned it into an automated digital tool. Piedmont further developed the tool and has now built it into the hospital’s electronic medical record, where it influences the ordering of retests.
A user can answer their “ifs” by clicking through questions, and the “if-this-then-do-that” algorithm makes recommendations for best courses of action, ranging from immediately treating a patient for COVID-19 to retesting to consulting a specialist. The final decision remains with the physician.
The questions are deceptively simple, but the recommendations are not always obvious. That reflects the algorithm’s usefulness to fill gaps in thinking about the new sickness, which can confront clinicians with surprises.
“If a patient has not had close contact with positive patients and the first test came back negative, a physician may think the patient does not need to be retested. But actually, the patient may need a second test because they are in intensive care and also have suspicious chest X-rays,” said Georgia Tech graduate research assistant April Yu, who converted the decision tree into a digital tool.
“One of our big worries in using a brand-new test like the coronavirus test is that it will miss real cases, and this tool helps prevent that,” said Dr. Bronwen Garner, who helped develop the original decision tree and is an infectious disease specialist at Piedmont Healthcare. “It also helps reassure physicians when they get a negative result that it is probably a true negative.”
Suspenseful decision-making
A physician’s reaction to an initial negative test can mean life or death because the physician not only decides on follow-up testing but also on treatment pathways and quarantine.
“If you make a misstep in the thought process, it can lead to cascading impacts not only for the patient but also for healthcare professionals and family members, who may be exposed to the patient,” said Pinar Keskinocak, William W. George Chair and Professor in Georgia Tech’s Stewart School of Industrial and Systems Engineering. “This tool is meant to help doctors easily stay on the decision tree path.”
Michael O’Toole, executive director of Piedmont Healthcare’s quality improvement department, originally pictured doctors getting an automated version of the decision tree to use on their phones. O’Toole called Keskinocak, and she tapped Yu, a member of her research group.
“Literally within four hours they had it ready for us. It was incredible,” said O’Toole, a Georgia Tech alumnus who studied industrial and systems engineering.
“It was a very pleasant surprise,” said Dr. Garner, who is also a Georgia Tech graduate. “Automated tools are better than a paper format because they’re in the same format as orders in our electronic system. We get notifications in real time instead of having to remember to check a piece of paper.”
The tool is in place in the system where doctors order retests and is specific to Piedmont’s workflow. It may not be directly transferable to other health care systems.
Piedmont Healthcare simplified the logic even more, and the hospital built its own custom alerts to guide physicians on retesting. For cases that are more ambiguous, Piedmont Healthcare’s final version of the tool also gives physicians inside the hospital guidance to consult with their in-house infectious disease specialists.
If-this-then-retest
In her original version, Yu had turned the decision tree criteria into a short panel of questions with yes and no answers. It took her six iterations to arrive at her final version.
Yu’s version asked whether the patient:
- has a relevant ailment
- previously tested positive for coronavirus
- is now in an intensive care unit
- has worsening lung conditions
- shows telltale lung damage in imaging
- has been diagnosed with a different ailment
- the patient has had contact with someone else who tested positive for coronavirus.
On the back end, the algorithm guided the user through risks of coronavirus presence based on the answers.
“The steps were easy to follow, and the answers were color-coded for urgency with white, yellow, and red,” said Keskinocak, who also directs Georgia Tech’s Center for Health and Humanitarian Systems.
One bright yellow answer read: “This patient needs re-testing 24 hours after the initial test!” And there were further recommendations on how to handle the case.
Here's how to subscribe to our free science and technology newsletter
Also read: Advice on DIY masks
Writer & Media Representative: Ben Brumfield (404-272-2780), email: ben.brumfield@comm.gatech.edu
Georgia Institute of Technology
Apr. 03, 2020
COVID-19 has caught Pinar Keskinocak well prepared. For years, she has studied how societies manage pandemics, and how outbreaks overtax the health care system and wrack supply chains to worsen pandemics. Here she shares her insights.
Empty classrooms and supermarket shelves marked the beginning of the COVID-19 pandemic. But Keskinocak expects more signs of the times to come – such as pop-up pandemic clinics and the shortage and rationing of medical supplies beyond masks and ventilators.
Keskinocak is the director of the Center for Health and Humanitarian Systems at the Georgia Institute of Technology, which studies how government and private sectors can cooperate to handle health and humanitarian crises. And she is William W. George Chair and Professor in Georgia Tech’s H. Milton Stewart School of Industrial and Systems Engineering.
In previous research, Keskinocak’s team created a model that accurately ran the course of the 1918 Spanish flu pandemic, and when COVID-19 struck, her team was already in the middle of modeling how special clinics could significantly slow a pandemic. In the meantime, temporary clinics in Wuhan, China, appear to have validated her model.
Healthcare expansion now
The surge of COVID-19 patients pushed Italy’s health care system into a very ugly crisis, and the U.S. needs to take measures now to handle similar patient surges. Pandemics often strike in two waves or more, and the second is usually the worst, so measures need to be lasting, Keskinocak said.
Even without COVID-19, the U.S. healthcare system has been under strain. Emergency rooms are often overcrowded; it takes a long time to schedule an appointment, and there is a chronic shortage of nursing staff.
[Read Keskinocak's guest op-ed in the New York Daily News: COVID clinics now]
“We need to expand capacity and unleash creative flexibility in our healthcare systems. We should use more telemedicine and create self-service stations for testing. I would particularly like to see specialized COVID-19 clinics established now,” Keskinocak said.
“Special clinics could be separate spaces in existing facilities or standalone facilities. As COVID-19 spreads, we expect a lot more people with cold- and flu-like symptoms to seek testing and care. The healthcare capacities are just not there for a business as usual approach, and taking it could harm patients by delaying care and increasing risk of infection.”
Gathering COVID-19 patients in tight spaces like waiting rooms with other patients would increase the coronavirus’ spread, and patients with preexisting conditions could face mortal threat. Contagion could also spread into hospitals.
“Dedicated pandemic clinics could implement targeted hygiene, air filtration, and specialized protective equipment beyond masks and gloves for healthcare workers. They can tailor workflows to test and care for patients quickly and effectively and keep them away from other patients and staff,” Keskinocak said.
Payment needs to be easy, too, including financing the uninsured. In the middle of a public health emergency, it is vital to not get bogged down by restrictions meant for normal times.
Potentially dangerous shortages
Toilet paper will make a comeback in supermarkets, but in its place, life-saving medications could become perilously scarce. Countries need to act now to prevent this from compounding the COVID-19 crisis.
“Dwindling availability of hospital beds, ventilators, and personal protective equipment like masks and gloves during a patient surge – those are the obvious things. But we could also see shortages of items like asthma medication or antidepressants. Worst case, even food supplies could run low,” Keskinocak said.
[Read Keskinocak's guest op-ed in The Hill: medical supply chain dangers]
Here’s how shortages work and can lead to price gouging and also rationing. The latter can have good effects.
“Shortages are the result of supply-demand imbalance caused by either an unexpected increase in demand or unexpected decrease in supply or both. Shortages are common in crises such as natural disasters or health emergencies. But given the worldwide slowdown of economic activity in pandemics, disruptions could get much worse this time,” Keskinocak said.
“Supply chains are actually intricate webs of multiple parts that span the globe. Pandemics damage many of those parts, and it can take time to recover. This creates a more serious and worrisome imbalance between supply and demand.”
Toilet paper will return because people fear-hoard it in a panic but consume it at normal rates. When the panic runs its course, demand slows back down to the actual rate of consumption and its normal supply chain, which is relatively simple, catches up.
“With medicine and healthcare services and supplies, the increase in demand is typically already in line with consumption, so a shortage in supply or increase in demand can create a supply-demand gap that continues for a long time,” Keskinocak said. “Medical supply chains are also very complex and fragile.”
Future vaccine distribution
In normal times, most supply chains work at a plodding pace, and when crisis strikes, it is tough to ramp them up due to expensive equipment, complex logistics, and strict regulations, particularly in health care. Even temporary shortages of medicines and medical devices can have consequences for patients who need them.
“If shortages become serious, rationing – with a priority allocation to those most in need – can help balance demand and supply for critical items like medications.”
Once created and approved, the production of vaccines or antivirals for COVID-19 will ramp up slowly and could be in short supply at first. Decision-makers need plan investments now in the supply chains necessary for their effective distribution.
This will include painful, necessary decisions like prioritizing first doses for healthcare workers, people with pre-existing conditions, and the elderly. The current system of restocking vaccines in the U.S. after initial distribution also has serious gaps that need fixing to save many more lives.
In the meantime, social distancing is one of the best ways to protect everyone and reduce the patient surge into clinics. Do it if you or anyone in your household has any cold-like symptoms.
[Read Keskinocak's commentary on social distancing on AJC.com]
Also read: Vaccine Supply Gaps Can Make Pandemics Deadlier
Media contacts: Ben Brumfield (ben.brumfield@comm.gatech.edu) and John Toon (john.toon@comm.gatech.edu)
Feb. 11, 2020
Four Georgia Institute of Technology faculty members have been elected as new members of the National Academy of Engineering (NAE). Marilyn Brown, Thomas Kurfess, Susan Margulies, and Alexander Shapiro join 83 other new NAE members for 2020 when they are formally inducted during a ceremony at the academy’s annual meeting on Oct. 4 in Washington, D.C.
Election of new NAE members, the culmination of a yearlong process, recognizes individuals who have made outstanding contributions to "engineering research, practice, or education, including, where appropriate, significant contributions to the engineering literature" and to "the pioneering of new and developing fields of technology, making major advancements in traditional fields of engineering, or developing/implementing innovative approaches to engineering education."
“It’s the honor of a lifetime to be recognized by the National Academy of Engineering for the impact we’ve have on understanding lung injuries in the critical care unit and traumatic brain injuries in children,” said Margulies, chair of the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University and, with Brown and Elsa Reichmanis (elected in 1995), one of just three women on the Georgia Tech faculty accorded NAE membership – one of the highest professional distinctions an engineer can receive.
“Our work is deeply collaborative, and I am grateful to the engineers, scientists, physicians, and patients who are partners in our journey,” Margulies added.
Margulies, a researcher in the Petit Institute for Bioengineering and Bioscience at Tech and a Georgia Research Alliance Eminent Scholar in Injury Biomechanics at Emory, was elected, “for elaborating the traumatic injury thresholds of brain and lung in terms of structure-function mechanisms,” according to the NAE announcement.
Using an integrated biomechanics approach, Margulies’ research program spans the micro-to-macro scales in two distinct areas, traumatic brain injury and ventilator-induced lung injury. Her work has generated new knowledge about the structural and functional responses of the brain and lungs to their mechanical environment. Margulies came to Georgia Tech in 2017 from the University of Pennsylvania, where she’d been a professor of bioengineering, and had earned her Master of Science in Engineering and Ph.D. in Bioengineering.
Brown is Regents and Brook Byers Professor of Sustainable Systems in the School of Public Policy. Her deep expertise in climate and energy policy helped shape numerous reports for the Intergovernmental Panel on Climate Change, including one that led to the organization receiving the Nobel Peace Prize in 2007.
She joined Georgia Tech in 2006 after a career at the U.S. Department of Energy's Oak Ridge National Laboratory, where she led several national climate change mitigation studies and became a leader in the analysis and interpretation of energy futures in the United States. Her research at Tech focuses on the design and impact of policies aimed at accelerating the development and deployment of sustainable energy technologies, emphasizing the electric utility industry. She was elected to NAE “for bridging engineering, social and behavioral sciences, and policy studies to achieve cleaner electric energy.”
Brown, who earned her Ph.D. at the Ohio State University, co-founded and chaired the Southeast Energy Efficiency Alliance, served two terms as a presidential appointee on the board of the Tennessee Valley Authority – the nation’s largest public power provider – and also served two terms on the U.S. Department of Energy’s Electricity Advisory Committee, where she led the Smart Grid Subcommittee.
“The most rewarding feature of my career has been working toward solutions with colleagues across disciplines,” Brown said.
Shapiro is the Russell Chandler III Chair and professor in the H. Milton Stewart School of Industrial and Systems Engineering, where his research is focused on stochastic programming, risk analysis, simulation-based optimization, and multivariate statistical analysis.
In 2013, he was awarded the INFORMS Khachiyan Prize for lifetime achievements in optimization. He received the 2018 Dantzig Prize from the Mathematical Optimization Society and the Society for Industrial and Applied Mathematics.
Since earning his Ph.D. in applied mathematics-statistics from Israel’s Ben-Gurion University of the Negev in 1981, Shapiro has made substantial contributions to the fields of optimization and large-scale, stochastic programming, and he was elected to NAE “for contributions to the theory, computation, and application of stochastic programming.”
Kurfess is professor and HUSCO/Ramirez Distinguished Chair in Fluid Power and Motion Control in the George W. Woodruff School of Mechanical Engineering, where he has helped guide the evolution of technology as a pioneer in the digital transformation of manufacturing.
Improving manufacturing technology is a pursuit that has roots in his childhood. “I grew up in my father’s machine shop,” said Kurfess, who has a special fondness for mom-and-pop operations. He was elected by the NAE “for development and implementation of innovative digital manufacturing technologies and system architectures.”
“I’m proud that the work we do has a positive impact on small and medium-sized enterprises, which are about 99% of the manufacturing operations, as well as large operations,” said Kurfess, who earned all of his degrees at MIT. “Our work targets people who are implementing the digital thread in manufacturing, and what the digital thread will do is make sure those smaller enterprises, those mom and pops, can have access to the latest and greatest technologies.”
Research News
Georgia Institute of Technology
177 North Avenue
Atlanta, Georgia 30332-0181 USA
Media Relations Contact: John Toon (404-894-6986) (jtoon@gatech.edu).
Writer: Jerry Grillo
News Contact
John Toon
Research News
(404) 894-6986
Feb. 11, 2020
Four Georgia Institute of Technology faculty members have been elected as new members of the National Academy of Engineering (NAE). Marilyn Brown, Thomas Kurfess, Susan Margulies, and Alexander Shapiro join 83 other new NAE members for 2020 when they are formally inducted during a ceremony at the academy’s annual meeting on Oct. 4 in Washington, D.C.
Election of new NAE members, the culmination of a yearlong process, recognizes individuals who have made outstanding contributions to "engineering research, practice, or education, including, where appropriate, significant contributions to the engineering literature" and to "the pioneering of new and developing fields of technology, making major advancements in traditional fields of engineering, or developing/implementing innovative approaches to engineering education."
“It’s the honor of a lifetime to be recognized by the National Academy of Engineering for the impact we’ve have on understanding lung injuries in the critical care unit and traumatic brain injuries in children,” said Margulies, chair of the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University and, with Brown, one of just three women on the Georgia Tech faculty accorded NAE membership – one of the highest professional distinctions an engineer can receive.
“Our work is deeply collaborative, and I am grateful to the engineers, scientists, physicians, and patients who are partners in our journey,” Margulies added.
Margulies, a researcher in the Petit Institute for Bioengineering and Bioscience at Tech and a Georgia Research Alliance Eminent Scholar in Injury Biomechanics at Emory, was elected, “for elaborating the traumatic injury thresholds of brain and lung in terms of structure-function mechanisms,” according to the NAE announcement.
Using an integrated biomechanics approach, Margulies’ research program spans the micro-to-macro scales in two distinct areas, traumatic brain injury and ventilator-induced lung injury. Her work has generated new knowledge about the structural and functional responses of the brain and lungs to their mechanical environment. Margulies came to Georgia Tech in 2017 from the University of Pennsylvania, where she’d been a professor of bioengineering, and had earned her Master of Science in Engineering and Ph.D. in Bioengineering.
Brown, a Regents and Brook Byers Professor of Sustainable Systems in the School of Public Policy, was co-recipient of the Nobel Peace Prize in 2007 (for co-authorship of the Intergovernmental Panel on Climate Change Working Group III Assessment Report on Mitigation of Climate Change, Chapter 6).
She joined Georgia Tech in 2006 after a career at the U.S. Department of Energy's Oak Ridge National Laboratory, where she led several national climate change mitigation studies and became a leader in the analysis and interpretation of energy futures in the United States. Her research at Tech focuses on the design and impact of policies aimed at accelerating the development and deployment of sustainable energy technologies, emphasizing the electric utility industry. She was elected to NAE “for bridging engineering, social and behavioral sciences, and policy studies to achieve cleaner electric energy.”
Brown, who earned her Ph.D. at the Ohio State University, co-founded and chaired the Southeast Energy Efficiency Alliance, served two terms as a presidential appointee on the board of the Tennessee Valley Authority – the nation’s largest public power provider – and also served two terms on the U.S. Department of Energy’s Electricity Advisory Committee, where she led the Smart Grid Subcommittee.
“The most rewarding feature of my career has been working toward solutions with colleagues across disciplines,” Brown said.
Shapiro is the Russell Chandler III Chair and professor in the H. Milton Stewart School of Industrial and Systems Engineering, where his research is focused on stochastic programming, risk analysis, simulation-based optimization, and multivariate statistical analysis.
In 2013, he was awarded the INFORMS Khachiyan Prize for lifetime achievements in optimization. He received the 2018 Dantzig Prize from the Mathematical Optimization Society and the Society for Industrial and Applied Mathematics.
Since earning his Ph.D. in applied mathematics-statistics from Israel’s Ben-Gurion University of the Negev in 1981, Shapiro has made substantial contributions to the fields of optimization and large-scale, stochastic programming, and he was elected to NAE “for contributions to the theory, computation, and application of stochastic programming.”
Kurfess is professor and HUSCO/Ramirez Distinguished Chair in Fluid Power and Motion Control in the George W. Woodruff School of Mechanical Engineering, where he has helped guide the evolution of technology as a pioneer in the digital transformation of manufacturing.
Improving manufacturing technology is a pursuit that has roots in his childhood. “I grew up in my father’s machine shop,” said Kurfess, who has a special fondness for mom-and-pop operations. He was elected by the NAE “for development and implementation of innovative digital manufacturing technologies and system architectures.”
“I’m proud that the work we do has a positive impact on small and medium-sized enterprises, which are about 99% of the manufacturing operations, as well as large operations,” said Kurfess, who earned all of his degrees at MIT. “Our work targets people who are implementing the digital thread in manufacturing, and what the digital thread will do is make sure those smaller enterprises, those mom and pops, can have access to the latest and greatest technologies.”
Research News
Georgia Institute of Technology
177 North Avenue
Atlanta, Georgia 30332-0181 USA
Media Relations Contact: John Toon (404-894-6986) (jtoon@gatech.edu).
Writer: Jerry Grillo
News Contact
John Toon
Research News
(404) 894-6986